Abstract
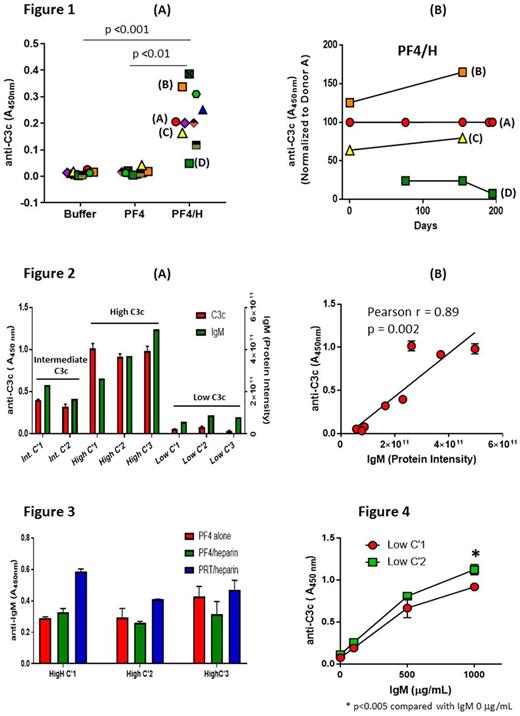
We recently described the early immunizing events following exposure to heparin that likely contribute to the development of Platelet Factor 4 (PF4)/heparin (H) antibodies leading to heparin-induced thrombocytopenia (HIT). In these studies, we demonstrated significant complement (C') activation by PF4/heparin complexes in vitro and in patients receiving heparin therapy, as well as selective binding of C'-coated antigen to B-cells via CD21 (Khandelwal, Blood 2016). To examine the mechanism underlying C' activation by PF4/heparin complexes, we developed a plasma-based capture immunoassay to detect complement activation fragment C3c bound to PF4/heparin complexes (ASH 2016, Abstract # 3734). In this assay, when plasma from healthy donors is incubated under identical conditions with buffer, PF4 alone or PF4/heparin, the degree of C' activation, as determined by antigen-bound C3c, varied significantly among healthy donors [Figure 1A, A 450nm (range): PF4/heparin = 0.05 -0.39 ; PF4 = 0.00- 0.04 ; buffer = 0.00-0.03; PF4/heparin v. PF4 (p<0.01); PF4/heparin v. buffer (p<0.001)]. The extent of C' activation for a given donor, categorized as high, intermediate or low (e.g., donor B=high, A&C=intermediate, and D=low C' activation in Figure 1A), remained stable over weeks to months (Figure 1B). To determine if phenotypic differences among donors were due to variability in levels of complement or complement regulatory proteins, we compared the plasma proteome of healthy donors with high (n=3), intermediate (n=2) or low (n=3) C' activation. Mass spectrometry analysis did not reveal differences in complement or complement regulatory proteins among donors tested. However, there was a marked correlation between donor phenotype and plasma IgM levels (Figure 2 A & B; r = 0.89, p = 0.002 by Pearson's correlation). We next examined the antigen specificity of IgM from donors expressing high C' activation phenotype. As shown in Figure 3, IgM binding was not antigen-specific, as IgM bound to PF4/heparin as well as to PF4 alone or PRT/heparin complexes. Based on data shown in Figures 2 & 3, we next asked if C' activation by PF4/heparin complexes in vitro reflects the total circulating level of IgM. To address this question, we added varying amounts of commercial IgM (0-1000 mcg/mL; Athens Research and Technology, Athens, Georgia) to the plasma of two donors with a low C' activation phenotype. As shown in Figure 4, increasing concentrations of IgM caused a dose-dependent increase in C' activation (> 10 fold of increase in anti-C3c (A450) at 1000 mcg/mL IgM compared to no IgM, p <0.005). Together, these studies indicate that low-avidity interactions between naturally-occurring IgM and PF4/heparin contribute to C' activation in plasma and likely mediated through the classical pathway. Differences in circulating IgM levels may contribute to susceptibility towards C' activation by PF4/heparin complexes and subsequent development of PF4/heparin antibodies in patients receiving heparin therapy. Our findings also hold promise for targeting the classical pathway as a strategy for preventing the development of HIT antibodies.
Cines: Syntimmune: Research Funding; Astellas: Consultancy; Rigel: Consultancy; T2 Biosystems: Research Funding; Amgen: Consultancy; Ionic: Consultancy; Juno: Consultancy. Arepally: Biokit: Patents & Royalties.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal